2024.05.07 Tuesday
Gut Bacteria Metabolite Shows Promise of Fighting Inflammatory Bowel Disease
Study highlights the molecular mechanisms underlying the anti-inflammatory effects of γKetoC, a gut bacteria-generated linoleic acid metabolite, using mice models

Gut microbiota or the population of microbial inhabitants in the intestine, plays a key role in digestion and maintenance of overall health. Any disturbance in the gut microbiota can, therefore, have a systemic impact. Intestinal microbes metabolize dietary components into beneficial fatty acids (FAs), supporting metabolism and maintaining host body homeostasis. Metabolites originating from polyunsaturated fatty acids (PUFAs), influenced by gut microbes such as Lactobacillus plantarum, exhibit potent effects on inflammation and immune responses. Manipulating gut bacteria and their metabolites shows promise in treating metabolic and inflammatory disorders. However, despite advances in gut health and wellness trends, the precise mechanisms governing the immunomodulatory properties of microbe-derived metabolites remain elusive.
To bridge this gap, a team of researchers led by Professor Chiharu Nishiyama from the Tokyo University of Science conducted a series of experiments using both in vitro and in vivo mouse models to understand how bacteria-generated FAs regulate immune responses. Explaining the rationale behind their work published in Frontiers in Immunology on 30 April, 2024, Prof. Nishiyama says, "PUFAs undergo metabolic transformations such as hydroxylation and saturation by enzymes possessed by intestinal bacteria. In recent years, a variety of beneficial physiological effects have been discovered for these intestinal bacterial metabolites. In this study, we have investigated the activity of multiple FA metabolites using mouse-derived immune cells."
To this end, the researchers used antigen-stimulated spleen cells to elicit an enhanced immune response. Subsequently, they investigated the impacts of different polyunsaturated fatty acid (PUFA) derivatives, focusing on metabolites of linoleic acid, a prevalent dietary fatty acid. Their findings revealed that KetoC, αKetoC, γKetoA, and γKetoC (enon derivatives of LA) markedly reduced the levels of interleukin 2 — a key protein that triggers the expansion of immune cells and inflammation. However, the original PUFAs in their unconverted form did not demonstrate the same immunosuppressive effects, emphasizing the critical role of bacterial conversion in activating their immunomodulatory properties. Furthermore, they observed that the enon (a functional group) FAs also suppressed prolonged T-cell proliferation and dendritic cell activation, which can lead to inflammation and autoimmune diseases. This anti-inflammatory effect was most pronounced with γKetoC. Hence, the researchers aimed to unravel the molecular mechanisms through which γKetoC exerted its immunosuppressive effects.
In addition, previous studies have shown the involvement of G protein-coupled receptors (GPCRs) and the transcription factor, NRF2, in anti-oxidant responses, which are mediated by several FA metabolites, whereas the involvement of GPCRs and NRF2 in the effects of γKetoC in dendritic cells was largely unknown. To clarify the role of these proteins in γKetoC-mediated immune responses, the researchers assessed the levels of inflammatory cytokines released from antigen-stimulated and γKetoC-treated dendritic cells. Their results suggested that γKetoC stimulated the NRF2 signaling pathway, which suppressed the production of inflammatory cytokines. Additionally, GPCR-signaling also inhibited inflammatory cytokine production in dendritic cells in an NRF2-dependent manner. This unveils a potential molecular axis governing the immunomodulatory effects of γKetoC.
To further validate their findings in vivo, the researchers used a mouse model of inflammatory bowel disease and examined immune and inflammatory responses by involving γKetoC treatment. They found that γKetoC treatment significantly reduced fibrosis-induced tissue damage in the colon, reduced colitis-induced weight loss, and improved stool scores. Furthermore, the treated mice showed decreased epithelial cell disruption and ulcers, along with reduced infiltration of immune cells and lower serum levels of inflammatory factors. Notably, the models that were deficient in NRF2 showed significant restoration of colitis-induced tissue damage following γKetoC treatment.
Overall, the present study sheds light on the potential mechanism by which γKetoC alleviates antigen-induced intestinal inflammation. Further studies are needed to understand the complex interplay between γKetoC, GPCR-signaling, and the NRF2 pathway, and uncover other potential targets of γKetoC which mediate its anti-inflammatory effects. Nevertheless, anti-inflammatory FA metabolites hold therapeutic promise in the treatment of intestinal inflammatory diseases and maintenance of gut health, as prebiotic or probiotic formulations. Sharing her concluding thoughts, Dr. Nishiyama states, "Our findings demonstrate that the compounds of dietary oils are converted into useful metabolites with anti-inflammatory effects by gut bacteria. By conducting detailed analyses at the individual, cellular, and genetic levels, we hope to understand how the food we eat daily influences the function of immune cells, and how these effects can be targeted for the prevention and mitigation of inflammatory diseases."
In summary, while the beneficial effects of bacterial PUFA metabolites were known, this study identified γKetoC as a metabolite playing a protective role in a colitis mice model. In the long run, these findings can help improve the quality of life for patients suffering from inflammatory diseases, and augment the possibility of developing functional foods, supplements, and nutraceuticals based on these microbial metabolites. Moreover, the researchers also speculate that these developments could help in the identification and development of compounds that are capable of preventing or alleviating immune-related diseases.
Here's wishing the team luck in their future research endeavors!
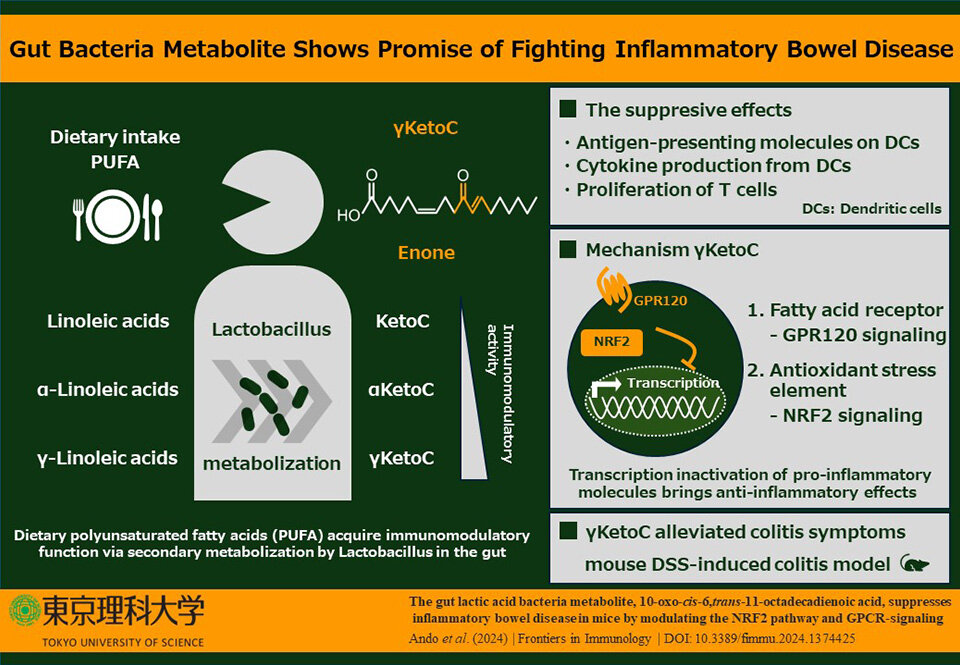
Image title: Gut bacteria metabolite holds potential in combating inflammatory bowel disease.
Image caption: Gut bacteria like Lactobacillus plantarum produce metabolites from polyunsaturated fatty acids, including the promising immunomodulator 10-oxo-cis-6,trans-11-octadecadienoic acid (γKetoC). It inhibits inflammation, CD4+ T-cell proliferation, and dendritic cell activation, potentially alleviating colitis symptoms, particularly in wild-type and Nrf2+/- mice.
Image credit: Chiharu Nishiyama from Tokyo University of Science, Japan
License type: Original Content
Usage restrictions: You are free to share and adapt the material. Attribution is required.
Reference
| Authors | : | Miki Ando1, Kazuki Nagata1, Ryuki Takeshita1, Naoto Ito1, Sakura Noguchi1, Natsuki Minamikawa1, Naoki Kodama1, Asuka Yamamoto1, Takuya Yashiro1, Masakazu Hachisu1, Gaku Ichihara2, Shigenobu Kishino3, Masayuki Yamamoto4, Jun Ogawa3, and Chiharu Nishiyama1 |
| Title of original paper | : | The gut lactic acid bacteria metabolite, 10-oxo-cis-6,trans-11-octadecadienoic acid, suppresses inflammatory bowel disease in mice by modulating the NRF2 pathway and GPCR-signaling |
| Journal | : | Frontiers in Immunology |
| DOI | : | 10.3389/fimmu.2024.1374425 |
| Affiliations | : |
1Department of Biological Science and Technology, Faculty of Advanced Engineering, Tokyo University of Science 2Department of Occupational and Environmental Health, Faculty of Pharmaceutical Science, Tokyo University of Science 3Division of Applied Life Sciences, Graduate School of Agriculture, Kyoto University 4Department of Molecular Biochemistry, Tohoku University |
About The Tokyo University of Science
Tokyo University of Science (TUS) is a well-known and respected university, and the largest science-specialized private research university in Japan, with four campuses in central Tokyo and its suburbs and in Hokkaido. Established in 1881, the university has continually contributed to Japan's development in science through inculcating the love for science in researchers, technicians, and educators.
With a mission of "Creating science and technology for the harmonious development of nature, human beings, and society," TUS has undertaken a wide range of research from basic to applied science. TUS has embraced a multidisciplinary research approach and undertaken intensive study in some of today's most vital fields. TUS is a meritocracy where the best in science is recognized and nurtured. It is the only private university in Japan that has produced a Nobel Prize winner and the only private university in Asia to produce Nobel Prize winners within the natural sciences field.
■
Tokyo University of Science(About TUS)

About Professor
Chiharu Nishiyama
from Tokyo University of Science
Chiharu Nishiyama is a Professor at the Faculty of Advanced Engineering, Department of Biological Science and Technology. She received her postgraduate degree in 1990 from the Department of Agricultural Chemistry at University of Tokyo Graduate School, followed by a Ph.D. from the University of Tokyo. Her areas of research interest include applied biochemistry, covering fields such as immunology, allergy, molecular biology, transcription factors, and cell development. Prof. Nishiyama has published over 130 research papers in international journals. She also received the prestigious JSBBA Award for Young Scientists in 2005, JSA Award for Young Scientists in 2005, and JAFI Award in 2019.
Laboratory website 
Official TUS website 
Funding information
This work was supported by a Grant-in-Aid for Scientific Research (B) 23H02167 (CN) and 20H02939 (CN); a Research Fellowship for Young Scientists DC2 and a Grant-in-Aid for JSPS Fellows 21J12113 (KN); a Scholarship for a Doctoral Student in Immunology (from Japanese Society for Immunology to NI); a Tokyo University of Science Grant for President's Research Promotion (CN); the Tojuro Iijima Foundation for Food Science and Technology (CN); a Research Grant from the Mishima Kaiun Memorial Foundation (CN); and a Research Grant from the Takeda Science Foundation (CN).

